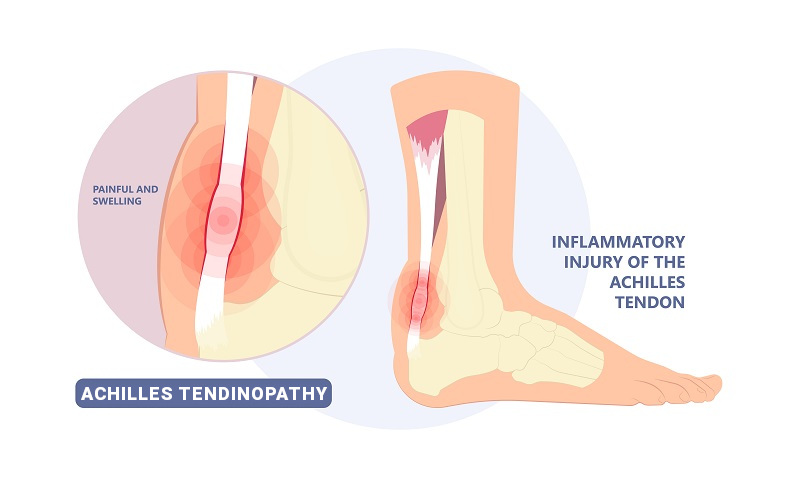
Achilles tendinopathy Achilles tendinitis, tendinosis, paratenonitis, enthesopathy, and insertional tendonitis are all among the terminology used to stratify different forms of chronic or acute Achilles tendon pain.
The Achilles tendon, also known as the Achilles heel cord, is considered the strongest tendon in the body. It consists of the tendinous portion of the combination of the muscle bellies of the calf muscles. There are two major muscles affiliated with the calf. The most prominent and visible exterior muscle group is known as the gastrocnemius. This is a heart-shaped muscle responsible for flexion of the foot, rapid power, and stepping movements. The second portion of this muscle group, is located slightly deeper to it, contributes to the Achilles tendon is the Soleus muscle. This muscle is responsible for stabilizing the lower leg during the gait cycle and a postural stance muscle when standing in place.
Disorders of the Achilles tendon frequently affect elite as well as recreational athletes,
often dubbed as “weekend warriors”. However, they can also affect the non-athletic and sedentary population for various systemic and metabolic reasons.
Causes of Achilles Tendon Pain
The reason behind this is that the Achilles tendon endures an enormous amount of pressure and strain frequently whenever walking, running, jumping, and sudden acceleration or deceleration such as jumping to reach a basketball hoop or tripping down a flight of stairs.
In the chronic setting and in sedentary or unhealthy individuals, overuse, vascular disease, peripheral neuropathy, rheumatologic, psoriatic, gout, reactive arthritis, Diabetes mellitus, lupus, ingesting a class of antibiotics called fluoroquinolones, repetitive steroid injections, or long term Systemic Steroid abuse can contribute to Achilles tendon degeneration or tendinosis; which is distinct from what the layman population frequently calls “tendinitis”, which is an acute inflammation of the Achilles tendon.
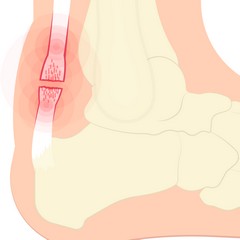
Chronic inflammation of the Achilles tendon produces a cellular biochemical process of oxidative stress. If not treated in time or adequately, this oxidative stress can eventually cause intrasubstance Achilles tendon degeneration, which leads to Achilles tendinosis. The hallmarks of this condition are a damaged, weak, inelastic, tight, scarred down, dysfunctional Achilles tendon.
There has been an estimation that almost 25% of competing athletes tend to suffer from Achilles tendinopathy over their lifetime. With 18% of this sustained by athletes younger than 45 years of age. Full-fledged Achilles tendon rupture happens in about 8.3% of competitive athletes. For runners especially, the lifetime incidence and occurance of Achilles Tendinopathy can go as high as 50%.
Treatment Options for Achilles Tendon Pain
The treatments available for acute Achilles tendinitis concentrate on reducing inflammation. This is done by protecting the tendon, resting it, immobilization through a cast or walking boot, gentle compression, elevation, icing, and oral anti-inflammatory medicine.
Because of the frequent repetitive overuse and micro traumatic damage to the tendon, a contracted tension develops which contributes to excessive scar tissue and pain.
This is why the cornerstone of treating Achilles tendinopathy consist of aggressive stretching.
This is why the cornerstone of treating Achilles tendinopathy consists of aggressive stretching. This can be done by a variety of manual stretching maneuvers, a course of physical therapy prescribed by a doctor, or a device that helps with stretching referred to as a night or a resting splint. In regards to stretching of the Achilles, a well-established way to stretch and fortify the tendon is through eccentric muscle strengthening, which can be further guided by physical therapists and the various modalities they have available for treatment.
In terms of shoe gear modification, orthotics with a heel lift in a soft and spacious heel counter can also help to accommodate swelling and deformity of the Achilles.
Steroid injections directly into the Achilles tendon are strongly discouraged because they can increase the risk for rupture.
Alternative Options to Treat Achilles Tendinopathy
However, injecting other products such as amniotic shot is an excellent alternative treatment option. Through the introduction of very specific cells called pluripotent cells this accomplishes four things:
- Reduction of pain
- Reduction of dense Inelastic scar tissue
- Anti-inflammatory
- Assist with tendon Regeneration
Other potential advanced modalities can include acoustic shockwave therapy. In an article published in 2020 in the Biomedical Research International Journal, data analysis of 66 patients with chronic Achilles tendinopathy, Shockwave Therapy was found to effectively relieve pain and improve the function of the hindfoot in patients with chronic Achilles’ tendinopathy. Especially in chronic cases, Shockwave therapy benefits Achilles disorders in functional improvement when patients use it as an Achilles tendon pain treatment.
Surgical Treatment for Achilles Tendinopathy
The last option includes surgical intervention. And depending on the extent and the location of the disease, the patient’s vascular status, and medical comorbidities, surgical intervention could include anything from tendon debridement and repair, minimally invasive or percutaneous repair, or full-fledge tendon takedown and approximation of frayed or damaged ends, and or reattachment back to the heel bone using tendon anchors. This option could entail anywhere from an 8 to 12-week recovery.
If you have more questions about disorders of the Achilles tendon, see your Certified Foot and Ankle Specialist today at a location near you.
Dr. Felipe Peterson, DPM, DABPM
Certified Foot and Ankle Specialist – St. Petersburg, Florida









