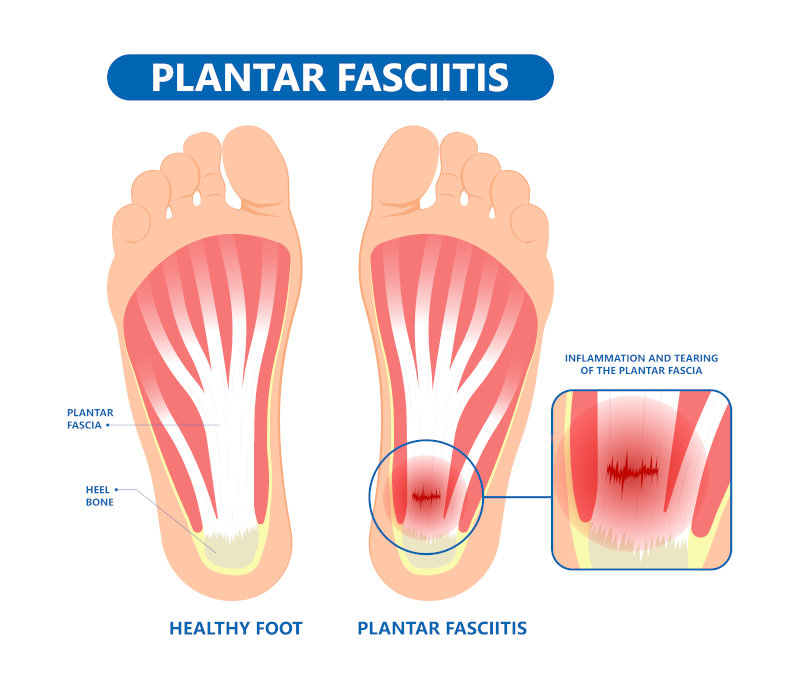
Plantar fasciitis is one of the most common causes of chronic heel pain. Many people have heard of heel spurs, but the spur itself is not the cause of the discomfort. The plantar fascia is a band of tissue on the bottom of the foot that attaches from the heel bone to the toes. Inflammation of the band typically causes great discomfort on bottom of the heel with the first few steps in the morning or when standing after long periods of rest. The pain can feel like stabbing or burning to the bottom of the heel or along the arch.
Symptoms of Plantar Fasciitis
Plantar fasciitis often manifests through distinctive symptoms that affect the feet, particularly the underside. Following are a few key indicators:
- Sharp Heel Pain: One of the hallmark symptoms of plantar fasciitis is a sharp, stabbing pain in the heel, especially when taking the first steps in the morning or after prolonged periods of rest. This pain can also intensify after standing or walking for extended periods.
- Pain Gradually Decreasing: While the pain can be severe initially, it often lessens as the foot limbers up with movement. However, it may return after long periods of standing or physical activity.
- Tenderness and Inflammation: The area around the heel where the plantar fascia connects to the heel bone can become tender to the touch. Inflammation may also be noticeable, leading to redness and swelling in some cases.
- Difficulty Bearing Weight: Plantar fasciitis can make it challenging to bear weight on the affected foot, particularly when standing, walking, or climbing stairs. The pain may feel like a deep ache in the heel.
- Pain Aggravation: Activities that involve repetitive movements or placing excessive strain on the feet, such as running, jumping, or standing for long periods, can exacerbate the pain associated with plantar fasciitis.
- Foot Discomfort: Beyond heel pain, individuals with plantar fasciitis may experience discomfort or aching along the bottom of the foot, extending towards the arch or even the toes.
Recognizing these symptoms early and seeking appropriate treatment, such as rest, ice therapy, stretching exercises, and possibly orthotic devices, can help manage plantar fasciitis and prevent it from becoming chronic or more debilitating.
 Causes of Plantar Fasciitis
Causes of Plantar Fasciitis
The causes of plantar fasciitis are varied. We know that certain foot types (flat feet and high arches), poor shoe choices, certain activities (running, dancing, etc), body weight, and profession can all contribute to heel pain.
There are many factors that could lead to plantar fasciitis developing in a patient:
- Overuse or Overload: Engaging in activities that put repetitive stress on the plantar fascia, such as running, dancing, or standing for long periods, can lead to micro-tears and inflammation.
- Foot Structure: Certain foot structures, like flat feet or high arches, can affect how weight is distributed on the feet, increasing the strain on the plantar fascia and making it more susceptible to injury.
- Improper Footwear: Wearing shoes with inadequate arch support, poor cushioning, or improper fit can contribute to plantar fasciitis by not providing proper support and alignment for the foot.
- Tightness and Weakness: Tight calf muscles or Achilles tendons, as well as weak foot and calf muscles, can alter the mechanics of the foot, leading to increased stress on the plantar fascia.
- Age and Activity Level: Plantar fasciitis is more common in middle-aged individuals and those who are physically active, as aging and repetitive activities can wear down the plantar fascia over time.
- Obesity: Excess body weight can put added pressure on the plantar fascia, increasing the risk of inflammation and injury.
Addressing these factors through proper footwear, stretching and strengthening exercises, maintaining a healthy weight, and gradually increasing activity levels can help prevent and manage plantar fasciitis.
Lesser-Known Risk Factors for Plantar Fasciitis
While common factors like foot structure, overuse, and improper footwear play a major role, there are other contributing factors that are often overlooked:
- Sudden Changes in Activity Level – A rapid increase in exercise intensity, such as jumping into a marathon training plan or starting a new high-impact workout, can shock the plantar fascia and lead to inflammation.
- Cold Weather and Stiffness – Colder temperatures can cause muscles and connective tissues, including the plantar fascia, to become tighter and less flexible, increasing the risk of strain and injury.
- Walking Barefoot on Hard Surfaces – While barefoot walking can strengthen foot muscles in some cases, doing so on hard floors—especially for long durations—can increase stress on the plantar fascia and heel.
- Poor Posture and Gait Issues – Alignment problems in the knees, hips, or lower back can change how weight is distributed across the feet, leading to excessive strain on the plantar fascia.
- Underlying Medical Conditions – Certain systemic conditions, such as rheumatoid arthritis, lupus, and diabetes, can contribute to chronic inflammation and increase the likelihood of plantar fasciitis.
By addressing these less obvious risk factors, individuals can take a more holistic approach to foot health, incorporating habits like proper warm-ups, postural corrections, and gradual activity changes to reduce the risk of plantar fasciitis.
Treatment options for Plantar Fasciitis
Treating plantar fasciitis traditionally involves a series of cortisone injections to the heel, calf stretches, oral anti-inflammatories, inserts, and a good supportive pair of sneakers. At Certified Foot & Ankle Specialists, we also offer amniotic injections for the most recalcitrant cases of plantar fasciitis. Amniotic injections deliver live human cells directly to the site of injury to reduce pain and inflammation and heal chronic soft tissue damage. These injections can also be used in refractory cases of Achilles tendinitis as well.
Minor surgical options
For the most severe and long-term cases of plantar fasciitis that have failed all conservative treatment, we do offer a minimally invasive procedure known as an endoscopic plantar fasciotomy which releases part of the plantar fascia to achieve immediate relief. The recovery is minimal and a patient can typically bear weight in just a couple of days.
It is not worth it to suffer from heel or ankle pain, so as soon as you see symptoms, make it a point to consult with your podiatrist. At all of our locations, we approach any conservative and comprehensive care with the same amount of importance. We are driven by excellence and will leave nothing short of the best care to help you get back on your feet.
A complete list of our podiatrists and their respective training and certifications can be viewed on their individual bio page. To make an appointment with a foot and ankle specialists near you, click here.
by Dr. Yanine Velasquez, DPM
Certified Foot and Ankle Specialist – Central Fort Myers, Florida