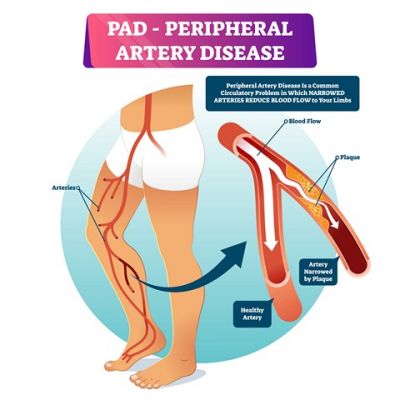
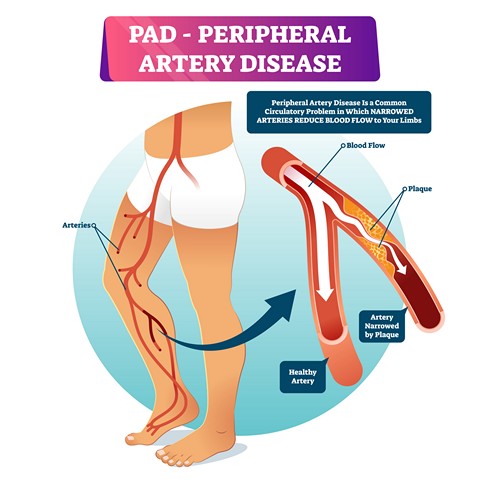
Peripheral Arterial Disease (PAD) most often occurs in the arteries of the feet and legs. The most common form of PAD is Atherosclerosis, commonly known as plaque, clogging or hardening of the arteries. This results in a decrease in blood flow to the feet and legs which can cause pain, delayed wound healing, and gangrene. PAD is associated with diseases such as Coronary Artery Disease (Heart Attacks), Stroke, High Cholesterol, High Blood Pressure and Diabetes. PAD can result in very serious, life threatening health concerns.
Risk factors for developing PAD include Age, High Blood Pressure, High Cholesterol, Smoking, Diabetes, Rheumatoid Arthritis, Family History, Sedentary Lifestyle, Unhealthy Diet, Psycho-Social factors, Obesity, and others. African Americans and Hispanic patients are at greater risk for PAD as well.
Symptoms include shiny skin on the feet and legs, lack of hair growth below the knee, pain in the feet, legs or thighs after walking a short distance or at rest, discoloration and/or slowly healing, often painful wounds on the legs or feet. If left untreated, PAD can result in the need for a major amputation of the foot or leg. This is most concerning because the life expectancy for 60% of PAD amputee patients is only 2 to 5 years.
Screening Recommendations
Considering the serious health effects associated with PAD, screening is indicated not only for those with symptoms, but also for all who have one or more of the risk factors mentioned above. This is important because 67% of patients are asymptomatic (have no symptoms) yet up to 20% of patients over 60, and over 5% of patients over 40 have PAD. The American College of Cardiology and American Heart Association released a joint practice guideline recommending screening in the following patient populations:
- Everyone Over Age 65
- Everyone Over 50 with Risk Factors
- Adults Younger than 50 with Diabetes and One Other Risk Factor
- American Diabetes Association also recommends Diabetics over 50 Undergo Annual Screening
Diagnosis
The diagnosis of PAD is initially made with a thorough history and physical exam performed by your doctor. Based on these findings, an ABI (Ankle Brachial Index) may be performed, which compares the blood pressure in your arm to your ankles. If these are not near equal, PAD may exist, and further testing is warranted with an Ultrasound and a specially trained vascular Ultrasonographer (technician).
An Arteriogram, MRA or CTA may then be performed to confirm the anatomy of the arteries and precisely locate any blockages. These techniques are typically performed in a specially equipped procedure room in the doctors office, hospital or surgery center or imaging center. Dye is injected into the arteries and multiple pictures are taken showing a roadmap of the arteries and any pathology.
Treatment
Fortunately, treatment is available for PAD if it is recognized and addressed in a timely fashion. For mild cases, exercise in combination with managing related conditions may be all that is required. Sometimes medication that helps with circulation may also be prescribed. In the painful or other advanced cases, such as those with poorly healing wounds, either endovascular or surgical procedures may be recommended to quickly restore blood flow to the feet and legs.
Endovascular Procedures – Fortunately, much progress has been made with these minimally invasive techniques. Similar to heart catheterization procedures, Doctors with advanced training are now able use devices such as stents in legs and feet to restore blood flow without surgery. In these cases, access to the arteries is gained through the groin, foot, leg \or wrist using a needle with no incision. Catheters are inserted through the needle, into the arteries under x-ray guidance. The doctor is then able to use special small tools to open clogged arteries, such as balloons (angioplasty), “roto-rooters” (atherectomy), stents or even perform a bypass by placing a stent outside the vessel to go around areas of severe blockage (SAFARI). These techniques are performed in a well-equipped Interventional Suite in an office or hospital, and patients are often able to return home the same day. Doctors who may be trained in these techniques include Interventional Cardiologists, Interventional Radiologists, or Vascular Surgeons.
Open Vascular Surgery – Should endovascular measures fail to restore blood flow in a PAD patient, traditional surgery may be performed. In these cases, performed in the hospital and usually requiring a short stay, the Vascular Surgeon works through standard, sometimes large open incisions to either remove plaque from vessels (endartarectomy) or bypass vessels using the patients veins harvested from the arms or legs, or synthetic vascular grafts. These procedures are associated with more pain and risk but are sometimes necessary in order to save one’s foot or leg.
As with any medical procedure, there can be no guarantees implied regarding outcomes with these types of procedures as there are risks involved. However, if conservative treatment fails to restore blood flow, the risks of refusing a procedure are often greater than the risks of having it performed. The goal should always be to save the foot or leg, if it remains functional, by using the least invasive, lowest risk means available. Our highly trained, multi-disciplinary team of doctors works together to save limbs for our patients every day.
Peripheral Arterial Disease
If you or someone you know would has been diagnosed with PAD, schedule an appointment with the board-certified podiatrists at Certified Foot & Ankle Specialists today.