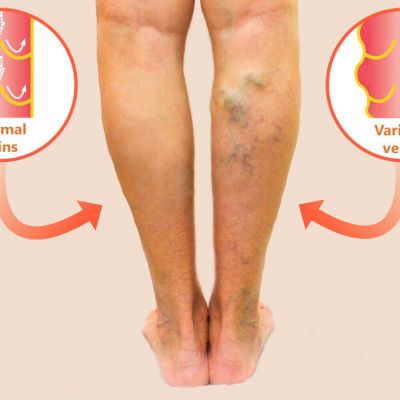
What is Venous Insufficiency?
Venous Insufficiency is a condition that results in swelling of the lower legs and is a result of underlying 'venous reflux'. This means that the blood is circulating from your heart, through the arteries down to your feet, but is not returning up through the veins as well as it should. In fact, ultrasound examination has confirmed that your veins are dilated and/or that the one-way valves inside your veins are not working properly. This is allowing the blood to regurgitate back down to your feet, ankles and lower legs causing swelling, discoloration, discomfort and eventually skin breakdown. Other systemic health conditions can result from venous insufficiency as well, including life threatening blood clots.
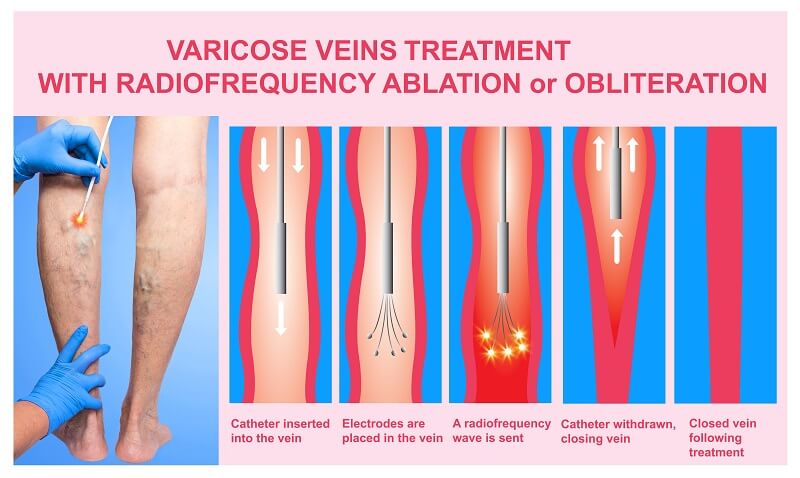
Endovenous Ablation Treatment or Radiofrequency Vein Ablation
Radiofrequency vein ablation has been reported to be highly effective treatment and has been recommended by your doctor to treat your venous insufficiency. This is a simple, in-office procedure performed under local anesthesia and ultrasound guidance. Using a needle and a special catheter, your doctor will close off the veins which are not working properly. This will cause the blood to circulate back up to your heart through the deeper veins that are working properly. Typically, patients notice a drastic reduction in swelling, disappearance of varicose veins, improvements in skin color and tone. There is usually minimal pain associated with this procedure. As with any procedure, there are risks involved and can be no guarantees regarding outcomes. Your doctor will review these risks with you and answer all of your questions prior to proceeding.
- You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to anesthetic medications, general anesthesia or to contrast materials containing iodine (sometimes referred to as “dye” or “x-ray dye”).
- Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners for a specified period of time before your procedure. Tylenol may be used if necessary.
Wear comfortable, loose clothing. You will need to remove all clothing and jewelry in the area under examination. - You should plan to have a relative or friend drive you home after your procedure.
- You may be asked to wear a gown during the procedure.
- Refrain from using moisturizers/lotions on the day of treatment.
- Be sure to eat a good breakfast and stay very well hydrated, refrain from caffeinated or decaffeinated beverages on the day of procedure.
- Bring compression stockings with you if you have them.
- There will usually be some bruising, swelling with minimal pain and discomfort after the procedure. Because of the appearance of the bruising and inflammation that often occurs in the treated area, you may be asked to wear thick supportive stockings or you may be wrapped with compression dressings.
- Inflammatory changes around the vein called superficial phlebitis may present as reddening of the skin, and minor local pain and tenderness.
- Most patients report relief of their symptoms (such as aching and swelling of the legs, and the appearance of the varicose veins) and are able to return to normal daily activities immediately, with little or no pain.
- Do not engage in any strenuous activity for the first 24 hours after the procedure.
- Do not take a bath for one to two days after the procedure; then you may shower.
- Walking 30–45 minutes each day for the duration of the treatment.
- Do not sit for prolonged periods and elevate your legs when you can for several days.
- A specially trained physician performs image-guided, minimally invasive procedures such as ablation.
- This procedure is often done on an outpatient basis.
- Your physician may first apply a numbing cream to the area over the abnormal vein to reduce discomfort.
- The doctor will clean, sterilize and cover the area with a surgical drape.
- Your doctor will numb the area where the catheter enters the abnormal vein with a local anesthetic. The doctor will use the ultrasound transducer to study the vein and track its path.
- A very small skin incision is made at the site.
- Using ultrasound guidance, the doctor inserts a catheter through the skin and positions it within the abnormal vein. The fiber or electrode is inserted through the catheter. The fiber or electrode tip is exposed by pulling the catheter back slightly.
- Local anesthetic is injected around the abnormal vein with ultrasound guidance. Energy heats the vein as the catheter is slowly withdrawn.
- Pressure will be applied to prevent any bleeding and the opening in the skin is covered with a bandage. No sutures are needed. A compression dressing or compression stockings may be applied.
- This procedure is usually complete within an hour.
* It is important to follow up as scheduled for post procedural ultrasounds to rule out blood clots and ensure the effectiveness of the procedure. Report to the ER and notify our office if you develop increasing swelling, redness, tightness in your legs or shortness of breath, chest pain or rapid heart beat.
Radiofrequency (RF) Vein Ablation
If you or someone you know show signs of varicose veins, call Certified Foot and Ankle Specialists to see a doctor who specializes in the treatment of venous disease in order to resolve this problem and return to your active lifestyle!