THE NUMBERS SPEAK FOR THEMSELVES
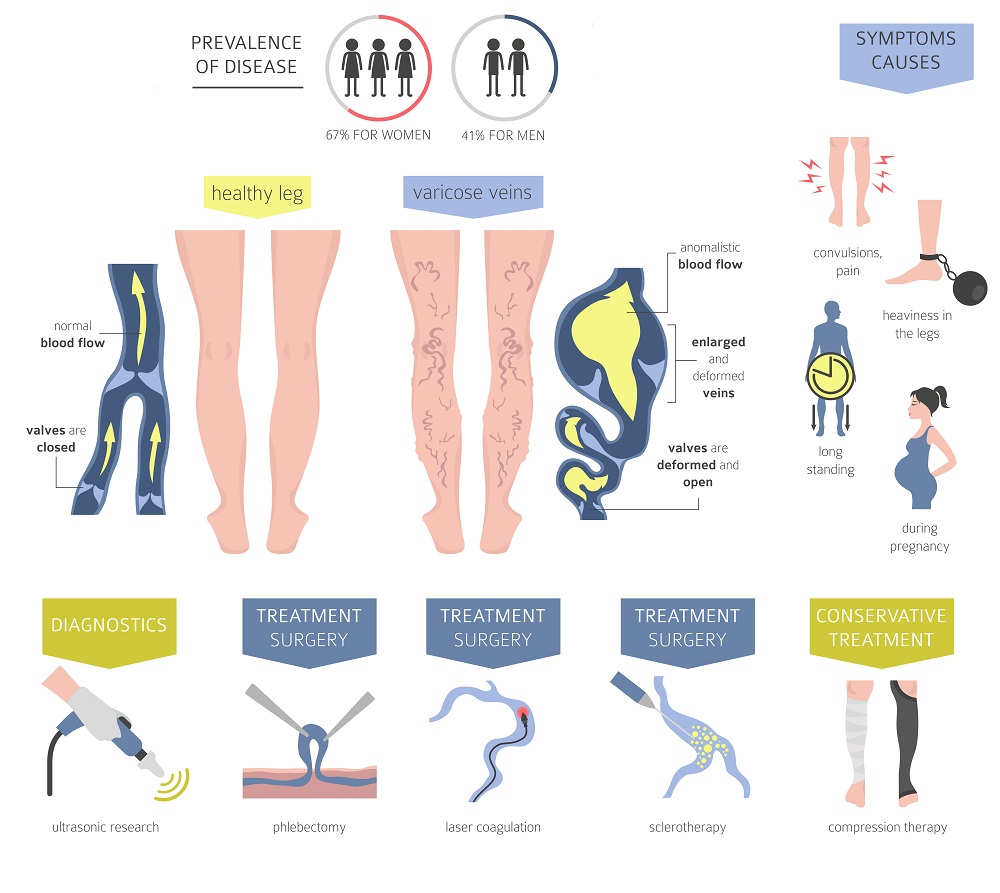
Venous insufficiency is a disease process which can affect all age groups. The older the group, the higher the prevalence. The overall prevalence of the disease is 25-40% for women and 10-20% for men. For any age group, women are more commonly affected than men. The annual occurrence rate is 6% and 1.9% for women and men, respectively. According to the Cleveland Clinic, 40% of people in the U.S. have venous insufficiency with varying degrees of symptomatology. There are an estimated 23 million cases of clinical venous insufficiency annually in the U.S. However, only 1.6 million people seek care for it during that time frame. Therefore, it is a common disease process that is under-treated.
Reasons of Venous Insufficiency
The reasons that venous insufficiency is under treatment are several. It is usually a slowly progressive disease process to which people commonly adapt. As both legs are usually involved, a normal leg for reference is lost and the symptoms may be considered to be the effect of aging, fatigue, arthritis or poorly supportive shoes. Only when surface varicosities appear or significant swelling of the lower legs occur do people tend to seek care. Primary care providers usually address other medical issues, however, ignore the signs or symptoms of venous insufficiency unless brought specifically to their attention by the patient. Symptoms are usually mild to moderate and addressing the problem may easily be put off by the patient.
THE CAUSES OF VENOUS INSUFFICIENCY
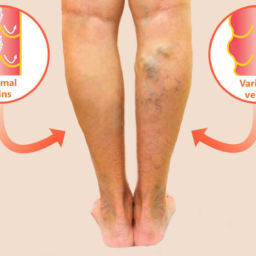
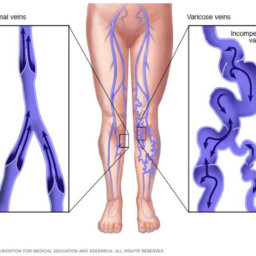
The cause of venous insufficiency is failure of one or more delicate one way valves in the veins which are designed to only allow blood to return to the heart and not let gravity pull the blood backwards to the lower leg and foot. Once one valve fails, it allows blood to flow backwards through the vein and puts more pressure on the next valve farther downstream, eventually causing it to fail and so on. Ultimately, venous blood is allowed to pool in the lower leg which congests the muscles, fat and skin and gradually causes inflammation, scarring and tissue breakdown.
Who’s at Risk? Factors That Increase the Chances of Venous Insufficiency
Several factors can increase the likelihood of developing venous insufficiency, ranging from genetics to lifestyle habits. A family history of varicose veins can predispose individuals to weakened vein walls and poor circulation. Pregnancy places extra pressure on the veins, making women more susceptible to the condition. Prolonged standing or sitting, especially on hard surfaces, can lead to poor blood flow, commonly affecting people in professions such as healthcare, retail, and factory work.
Certain high-impact sports, like soccer, long-distance running, and basketball, may contribute to vein damage due to repetitive strain and increased pressure in the legs. Hormone replacement therapy and birth control pills can also play a role, as hormones influence vein elasticity and circulation. Leg trauma or previous surgeries, particularly those involving the veins, may impair proper blood flow, while a history of deep vein thrombosis (DVT) increases the risk of chronic venous issues. Additionally, excess body weight places extra stress on the veins, potentially leading to circulation problems over time.
Understanding these risk factors can help individuals take proactive steps to maintain vein health and prevent complications associated with venous insufficiency.
The Role of Exercise in Managing Venous Insufficiency
Staying active is one of the most effective ways to improve circulation and manage symptoms of venous insufficiency. Regular movement helps strengthen the muscles in your legs, which act as a natural pump to push blood back toward the heart, reducing swelling, discomfort, and the risk of complications.
Best Exercises for Venous Insufficiency
- Walking: A simple yet powerful way to improve circulation, walking encourages the veins to work efficiently without putting too much strain on the legs. Aim for at least 30 minutes of brisk walking most days of the week to keep your blood flowing and prevent stagnation.
- Leg Elevation Exercises: Elevating your legs while lying down and performing ankle pumps or gentle leg lifts can help blood move back to the heart, reducing pressure in the veins and alleviating swelling.
- Calf Raises: Standing on your toes and then slowly lowering your heels strengthens the calf muscles, which play a crucial role in venous return. This exercise can be done multiple times a day, even while standing at work.
- Low-Impact Cardio: Swimming and cycling are great alternatives for those who want to stay active without putting excess stress on the veins. These activities promote circulation while being gentle on the joints and vascular system.
- Yoga and Stretching: Poses that elevate the legs, such as “Legs Up the Wall” or gentle stretching routines, can help reduce swelling and improve venous return.
Additional Support: Compression Therapy
In addition to exercise, wearing graded compression hose can provide external support to the veins, helping blood move more efficiently and preventing symptoms from worsening. Compression stockings come in various strengths, and a healthcare provider can help determine the best option based on individual needs.
SIGNS AND SYMPTOMS OF VENOUS INSUFFICIENCY
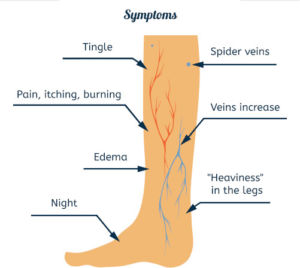
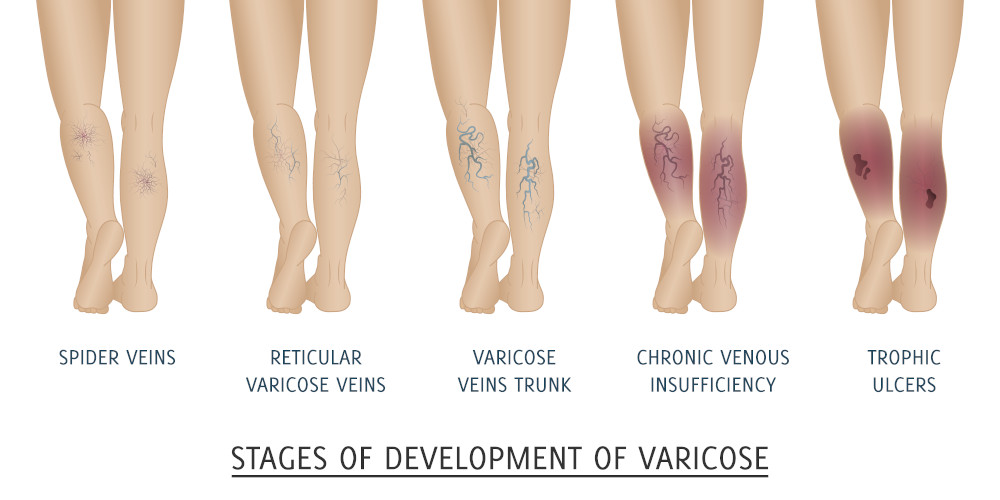
The signs and symptoms of venous insufficiency are initially subtle and usually progress slowly. The problem has never been demonstrated to spontaneously improve or resolve without treatment. Symptoms may include lower leg aching, heaviness, tightness, fatigue, itching, burning, restlessness, and cramping. Nocturnal leg cramping and restlessness are common. The symptoms, as well as lower leg edema usually worsen the longer the person is upright, either seated or standing, and are usually improved with elevation of the legs.
Signs of venous insufficiency in progression of severity include:
- small telangiectasia (spider veins)
- varicose veins (>2mm in diameter)
- ankle or leg swelling
- light blue foot or toes when legs are down which color improves with elevation of the legs
- skin changes of the lower leg including redness
- dry scaling skin
- brown permanent discoloration
- open non-healing sores (ulceration) .
PROGRESSION of venous insufficiency
Signs of venous insufficiency in progression of severity include small telangiectasia (spider veins), varicose veins (>2mm in diameter), ankle or leg swelling, light blue foot or toes when legs are down which color improves with elevation of the legs, skin changes of the lower leg including redness, dry scaling skin, and brown permanent discoloration, open non-healing sores (ulceration) .
HOW CAN WE TREAT VENOUS INSUFFICIENCY
Treatment options include:
- graded compression hose
- closure of the failed veins with irritating FDA approved medicine injections under ultrasound guidance (sclerotherapy/Varathena)
- catheter based closure using light energy (endovenous laser therapy or EVLT)
- radiofrequency ablation using high frequency radio waves, both essentially cauterizing closed the inside lining of the failed vein.
The catheter is inserted through an IV in the failed vein. Only local anesthetic is used for the procedure and there is no recovery or down time afterward. Mild post procedure discomfort is improved or resolved with regular walking and or Acetominophen (Tylenol) or Ibuprofen (Motrin). A thigh length compression stocking is worn for 5 to 14 days after the procedure depending on the procedure utilized. Improvement of the symptoms is usually within a week.
Certified Foot and Ankle Specialists are keenly aware of vein disease and have both the equipment and an American Board Certified cardiovascular specialist who is educated in the diagnosis and treatment of vein and all vascular diseases. We would be happy to evaluate and treat any vascular problems from which you may suffer.
By Dr. Randall Orem, DO, FACC,FSCAI.
Certified Foot and Ankle Specialists