About the Author: Dr. Ashley Bowles ,DPM, FACFAS
Board-certified podiatrist with experience treating foot and ankle conditions. Fellowship-trained in minimally invasive foot surgery and conservative treatment approaches. Member of the American Podiatric Medical Association and specializes in biomechanical foot disorders.
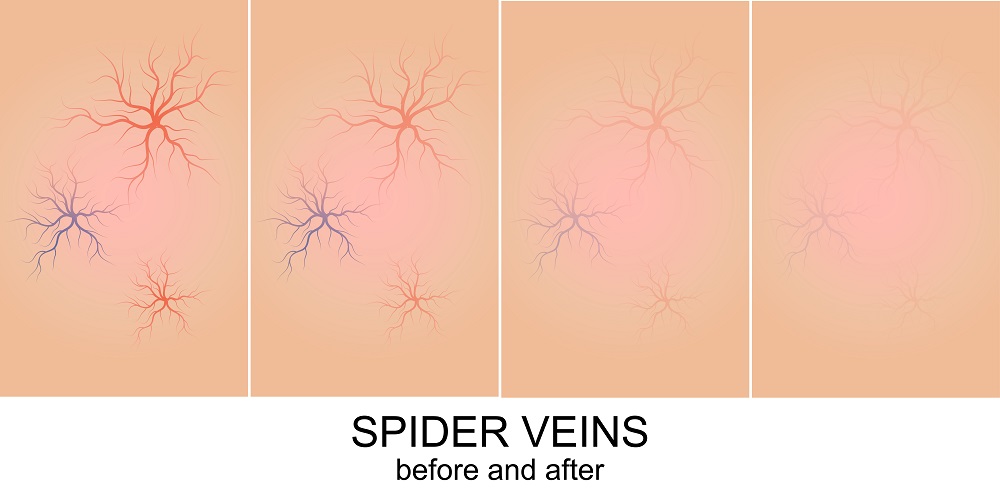
What are spider veins exactly?
Spider veins on the ankles and feet are small, visible veins that appear close to the surface of the skin. They are also known as telangiectasias and are usually blue, red, or purple in color. Spider veins occur when the valves within the veins stop functioning correctly, causing blood to pool in the veins and creating a visible web-like pattern on the skin. They are commonly seen in women, particularly during pregnancy or with aging, and can be caused by genetics, prolonged standing, obesity, and hormonal changes. Spider veins are generally harmless but can cause discomfort or aching in some people.
Are Spider Veins More Common in Men or Women?
Yes, spider veins are more common in women than in men. According to the American Society of Plastic Surgeons, up to 55% of women may develop spider veins at some point in their lives, while only about 45% of men are affected. This may be due to hormonal changes that occur during pregnancy, menopause, or with the use of certain birth control methods. Additionally, women tend to have a higher proportion of body fat than men, which can put additional pressure on the veins and increase the risk of developing spider veins. Other risk factors for spider veins include genetics, aging, obesity, and a history of blood clots. While spider veins are more common in women, men can still develop them and may benefit from treatment options such as sclerotherapy or laser therapy.
Symptoms of Spider Veins on Ankles and Feet: What You Need To Know
Spider veins are usually harmless and do not cause any symptoms. However, some people may experience discomfort or pain in the affected area. Spider veins are small, visible blood vessels that appear close to the surface of the skin. They often look like a spider web or tree branch, and can be red, blue, or purple in color. They can occur anywhere on the body, but are most commonly seen on the ankles, feet, and legs.
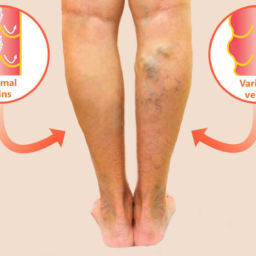
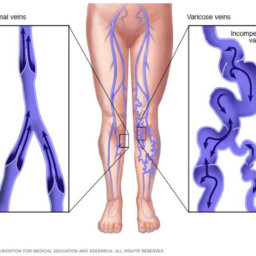
Spider veins are caused by increased pressure in the blood vessels, which can be caused by a variety of factors, including genetics, hormonal changes, obesity, and prolonged standing. They can also be a symptom of a more serious condition, such as chronic venous insufficiency. This typically happens when the valves within the veins do not perform or function properly. They in turn cause blood to pool in the veins and ultimately leading to the development of varicose veins and spider veins.
If you are experiencing pain, discomfort, or any other symptoms in the affected area, it is important to consult with a healthcare professional to determine the underlying cause and appropriate treatment options.
How Can You Prevent Spider Veins?
Preventing spider veins on the feet and ankles can be achieved by following some simple lifestyle changes:
- First and foremost, it is important to maintain a healthy weight and exercise regularly to improve circulation.
- If you need to stand for long periods of time, try taking breaks and walking around periodically to avoid putting excessive pressure on your feet and ankles.
- Additionally, wearing compression stockings can help improve blood flow and reduce the risk of developing spider veins.
It is also important to treat varicose veins promptly, as these are closely related to the symptoms of spider veins and can increase your risk of developing them. If you have a family history of spider veins or varicose veins, you may be at a higher risk of developing them yourself. In this case, it is especially important to take steps to prevent their development, such as regular exercise and wearing compression stockings.
Treatment Options for Spider Veins
There are several treatment options available for spider veins, which are small, visible blood vessels that appear close to the skin’s surface. These veins are usually harmless, but if left untreated, they can lead to complications such as blood clots or ulcers. Treatment options for spider veins include:
- Sclerotherapy: This involves injecting a solution into the affected vein, causing it to collapse and eventually fade from view.
- Laser therapy: This involves using a laser to target the affected vein, causing it to fade from view.
- Endovenous laser therapy: This is a minimally invasive procedure that involves using a laser to close the affected vein from the inside.
- Radiofrequency ablation: This is a minimally invasive procedure that uses radiofrequency energy to close the affected vein.
- Compression stockings: Wearing compression stockings can help improve blood flow and reduce the appearance of spider veins.
- Lifestyle changes: Making lifestyle changes such as exercising regularly, maintaining a healthy weight, and avoiding prolonged periods of standing or sitting can help prevent the development of spider veins.
It is important to note that while these treatments can help reduce the appearance of spider veins, they do not guarantee that new ones will not develop in the future. Spider and reticular veins are often a cosmetic concern, but those with symptomatic varicose veins or corona phlebectatica should see a phlebologist. Our boca raton vein specialists at Certified Foot and Ankle Specialists offer comprehensive evaluation, including a duplex venous ultrasound to assess for blood clots, blockages, and venous reflux.
We urge you to make an appointment with our vein care expert phlebologist so they can determine the best course of treatment for your individual needs, as well as to identify any underlying conditions that may be contributing to the development of spider veins.
FAQ: Spider Veins on Ankles and Feet
What are spider veins on legs?
Spider veins are small, visible blood vessels that appear close to the skin’s surface in web-like patterns. Also called telangiectasias, they typically appear red, blue, or purple and develop when tiny valves inside veins stop working properly, causing blood to pool.
They affect up to 55% of women and 45% of men and are generally harmless, though primarily a cosmetic concern. Common causes include genetics, hormonal changes, prolonged standing, obesity, and aging.
What causes spider veins on ankles?
Spider veins on ankles develop due to:
- Gravity and pressure: Ankles bear maximum pressure from blood pumping upward against gravity
- Weakened vein valves: When valves malfunction, blood pools and creates visible veins
- Genetics: Family history significantly increases risk
- Prolonged standing: Extended time on the feet increases leg vein pressure
- Hormonal changes: Pregnancy, menopause, and birth control
- Weight and aging: Extra weight and weakening vein walls over time
Why do spider veins appear around ankles?
Ankles are a common location because:
- They experience the strongest gravitational pull in your circulatory system
- Maximum blood pressure concentrates at this lowest point
- Skin naturally thins with age, making vessels more visible
Important note: When spider veins cluster in a fan pattern around ankles (corona phlebectatica), this can indicate more serious underlying venous problems and should be evaluated by a specialist.
Are spider veins on feet dangerous?
Spider veins are usually not dangerous—most people have no symptoms beyond visible veins. However, they can sometimes signal underlying issues.
Seek medical evaluation if you experience:
- Pain, aching, or burning
- Swelling or leg heaviness
- Skin discoloration or changes
- Itching or throbbing
- Cluster pattern around ankles (corona phlebectatica)
At Certified Foot and Ankle Specialists, we perform duplex venous ultrasound to check for blood clots, blockages, and venous reflux to ensure no underlying vein conditions exist.
What are dark veins on feet?
Dark veins can indicate two different conditions:
1. Visible spider/varicose veins: Dark blue, purple, or red veins showing through the skin
- Blue/dark blue: Vein is deeper beneath the skin
- Red/purple: Vein is very close to the surface
2. Venous stasis dermatitis: Dark brown pigmentation from chronic venous insufficiency
- Caused by iron deposits from broken-down blood cells
- Usually appears on the inner ankles first
- May indicate poor blood return to the heart
See a specialist if you notice:
- Sudden dark pigmentation
- Skin becoming hard, cracked, or scaly
- Spreading discoloration
- Open sores or wounds
Are spider veins on legs painful?
Most people experience no pain—spider veins are typically just a cosmetic concern. However, some report:
- Mild discomfort or aching
- Burning or itching
- Leg heaviness or fatigue
- Restless legs
- Mild swelling
Pain may indicate: Underlying venous insufficiency or progression to varicose veins. Consult a specialist if pain is persistent or interferes with daily activities.
How can I prevent spider veins?
While you can’t completely prevent spider veins (especially with genetic predisposition), you can reduce risk:
- Maintain a healthy weight: Reduces pressure on the veins
- Exercise regularly: Walking, swimming, cycling, to improve circulation
- Take breaks: Avoid prolonged standing or sitting
- Wear compression stockings: Improves blood flow
- Elevate legs: When resting, raise legs above heart level
- Treat varicose veins promptly: Prevents additional spider vein formation
What treatments are available?
Our vein specialists at Certified Foot and Ankle Specialists offer a comprehensive evaluation, including duplex venous ultrasound, to identify underlying conditions and recommend appropriate vein treatment such as radiofrequency vein ablation, sclerotherapy injections, or open vascular surgery.
When to schedule a consultation:
- Symptomatic spider veins (pain, burning, discomfort)
- Corona phlebectatica (ankle cluster pattern)
- Cosmetic concerns affecting quality of life
- Family history of venous disease
Contact Certified Foot and Ankle Specialists to schedule an appointment at our Boca Raton location or other offices throughout Florida.