Varicose veins, a common condition affecting millions globally, often manifest as visible vein swelling on the surface of the skin. Characterized by twisted and enlarged veins, this condition is not only a cosmetic concern but also an indication of underlying venous disease. This blog explores the stages of varicose veins, emphasizing the significance of early diagnosis and comprehensive treatment options to prevent disease progression and ensure optimal leg health.
Symptoms and Causes
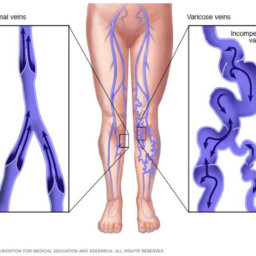
Symptoms of varicose veins include vein swelling visible on the surface of the skin, a heavy feeling in the legs, itching around one or more of your veins, and skin discoloration. The primary cause of varicose veins is the weakening of vein walls and valves, leading to chronic venous insufficiency where blood flow is hindered, and blood pools in the veins. Factors contributing to this condition range from genetic predisposition to extended periods of standing or sitting.
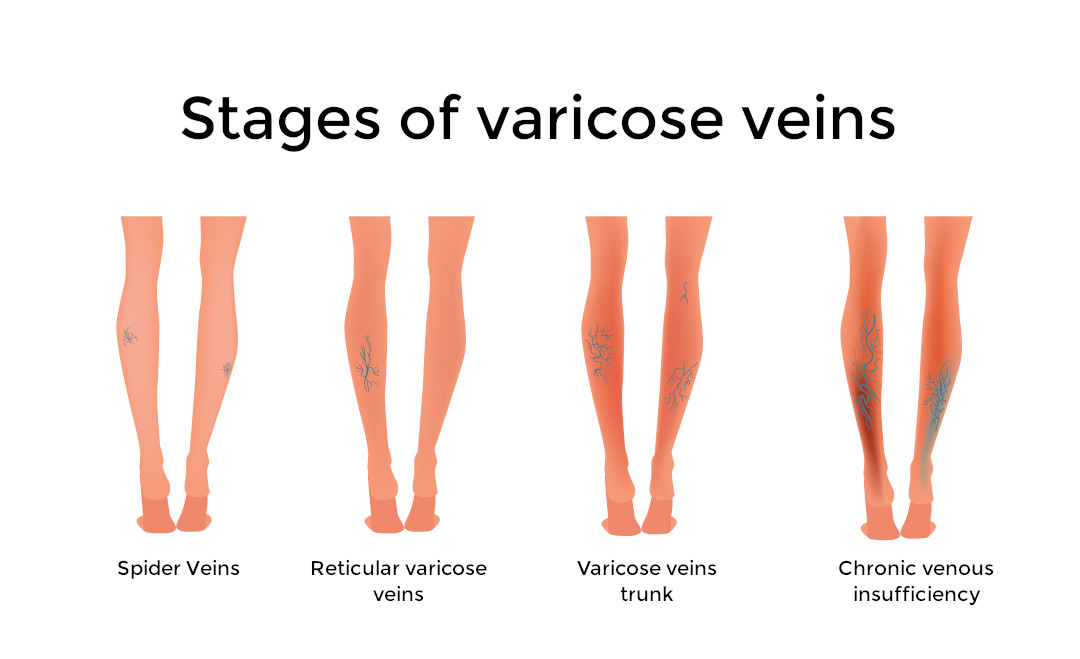
Stages of Varicose Veins
The progression of venous disease through its stages begins with minor symptoms, such as spider veins, which are small, damaged veins that can appear on the surface of the legs. As the condition worsens, patients may develop varicose veins, marked by more significant vein swelling and discomfort. Advanced stages include chronic venous insufficiency, leading to skin discoloration, venous ulcers, and the risk of blood clots.
Diagnosis
The diagnosis of the stages of varicose veins or venous insufficiency involves a comprehensive evaluation by a healthcare professional, typically a vascular specialist or a podiatrist at clinics like Certified Foot and Ankle Specialists.
- The process starts with a physical examination, focusing on the legs’ appearance, skin discoloration, and any signs of swelling or ulceration.
- A detailed medical history helps identify risk factors, such as family history of venous disease, obesity, and periods of prolonged standing or sitting.
- Advanced diagnostic tools include Duplex Ultrasound, a non-invasive imaging test that visualizes the blood flow and the structure of the leg veins. This test assesses the veins’ function, identifies any blood clots, and determines the extent of blood flow obstruction.
- In certain cases, additional imaging tests may be recommended to provide a comprehensive view of the venous system and to plan the most effective treatment strategy.
Surgical and Non-surgical Treatments for stages of Varicose Veins
Treatment options for varicose veins range from conservative measures to more invasive surgical procedures, depending on the severity of the condition and the individual’s overall health. Non-surgical treatments focus on alleviating symptoms and preventing further progression of the disease. These include compression stockings to improve blood flow, lifestyle modifications such as weight management and regular exercise, and sclerotherapy for smaller veins where a solution is injected to close off the veins.
For more advanced cases or when non-surgical treatments are ineffective, surgical options may be considered. These include endovenous laser therapy (EVLT) and radiofrequency ablation (RFA), minimally invasive procedures that use heat to seal off affected veins, and vein stripping, a traditional surgery to remove large varicose veins. Each treatment plan is tailored to the individual’s specific needs and the stages of varicose vein development.
Exercise
Regular physical activity is essential in managing varicose veins and preventing their progression. Exercise improves blood flow and strengthens the venous system, reducing the risk of chronic venous insufficiency. Effective exercises for individuals with varicose veins include walking, cycling, and swimming, which promote leg movement without excessive strain. Additionally, leg elevation and avoiding prolonged periods of standing or sitting can help minimize symptoms and improve blood circulation.
Preventative Measures
Preventing the progression of varicose veins involves a combination of lifestyle changes and proactive measures designed to improve venous health and reduce the risk of chronic venous insufficiency. By implementing these strategies, individuals can significantly impact their overall vein health and quality of life.
Maintain a Healthy Weight
- A high body mass index or BMI results in higher pressure being placed on the veins of your body. Our blood collects in the legs due to gravity and excess weight compounds the problem. Maintaining a healthy weight through a balanced diet and regular exercise can reduce this pressure and prevent the worsening of varicose veins.
Regular Physical Activity
- Engaging in regular exercise not only helps in weight management but also improves circulation. Activities that involve leg muscles, such as walking, swimming, and cycling, are particularly beneficial in promoting blood flow back to the heart and reducing blood pooling.
Proper Leg Elevation
- Elevating the legs above the heart level, especially after long periods of standing or sitting, can help blood flow more easily back to the heart, reducing the pressure in leg veins and minimizing the risk of vein swelling and varicose veins.
Wearing Compression Stockings
- Compression stockings apply gentle pressure to the legs, which can prevent blood from pooling in the leg veins and help the muscles and veins move blood more effectively. These are especially recommended for individuals who are predisposed to venous problems or who spend extended periods on their feet.
Avoid Prolonged Periods of Standing or Sitting
- Changing positions regularly and taking short walking breaks can help mitigate the adverse effects of prolonged standing or sitting. This simple measure encourages blood circulation and decreases the likelihood of blood pooling in the lower extremities.
Healthy Lifestyle Choices
- Smoking cessation and reducing alcohol intake can also positively affect venous health. These lifestyle choices can improve blood flow and reduce the risk of complications associated with varicose veins, such as venous ulcers and blood clots.
Implementing these preventative measures can significantly reduce the risk of developing varicose veins or prevent existing ones from worsening.
In summary, varicose veins are not merely a cosmetic concern but a sign of underlying venous disease that can progress to serious health issues if left untreated. Understanding the symptoms, causes, and stages of venous insufficiency is crucial for early detection and effective management. At Certified Foot and Ankle Specialists, we emphasize the importance of a comprehensive approach to diagnosing and treating varicose veins, incorporating both advanced medical interventions and simple lifestyle adjustments. Surgical and non-surgical treatments, alongside prescribed medications and recommended exercises, play a pivotal role in alleviating symptoms and preventing further complications.
Remember, early intervention and consistent management are key to maintaining healthy blood flow and preventing the progression of venous disease. If you’re experiencing symptoms or have concerns about varicose veins, we encourage you to seek professional medical advice to explore the best treatment options tailored to your condition.
Call Our Foot And Ankle Specialists today!
We have locations in the South East and West Coast of Florida to serve you better. If you are seeking a podiatrist in Fort Myers, look no further as we have certified doctors in Cape Coral and Central Fort Myers. Living on the East Coast? With locations in Broward and Palm Beach Country we have several locations to choose from.
Please contact us today at 855-550-3338 or send us a message to schedule a consultation.
As we strive to provide the highest standard of care for our patients, Certified Foot and Ankle Specialists remain committed to advancing treatment methodologies and educating the community on the importance of leg health. Together, we can work towards preventing the onset and escalation of varicose veins, ensuring a healthier, more active future for everyone.