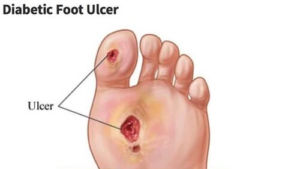
Patients with diabetes can be at risk for diabetic foot ulcers, infections, and complications from those infections. Diabetic foot ulcers or wounds put patients at a higher risk of hospitalization and need for surgery or amputation. In fact, according to the CDC, there are 130,000 hospitalizations a year for amputations in those with diabetes. Up to 11.8% of those with diabetes have a wound and many may go on to need surgery. This means that wound care for diabetic foot ulcers as well as prevention is of the utmost importance.
As physicians, we have to use our resources and work with patients in order to heal diabetic foot wounds to prevent such complications. If a patient also has numbness in their feet, they may not feel a foot wound developing. Diabetic foot sores that start from a small scrap or cut can unknowingly form into a deep ulcer. Checking your feet and keeping your blood sugar
Whether you have diabetes or are caring for a loved one requiring foot diabetic wound treatment, Certified Foot and Ankle Specialists can effectively help your wound heal and prevent further complications. Here we will discuss diabetic foot care and how to minimize the traumatic consequences of ulcers.
How do we care for diabetic foot wounds and how does one clean a diabetic foot wound?
Diabetic foot wound care focuses on creating a healthy environment in the wound in order for new skin cells to migrate across the wound. This often involves keeping the wound slightly moist. However, if the wound becomes too moist, due to excessive draining from the inside of the wound, you might require a more absorptive dressing.
For proper wound care, clean the wound with saline, apply a topical gel or antibiotic ointment medication to the wound once a day, as recommended by your doctor.
Sometimes certain ointments can help treat wounds that are covered in fibrous, yellow matter much like a burn wound. Other ointments for diabetic foot wounds include topical antibacterial ointments or creams that can be applied to help keep the wounds clean.
After cleansing the wound and applying the ointment, it is best to wrap the wound with a clean gauze dressing.
Keep the wound covered and moist
Our mothers may have told us that “airing out” a wound would help it heal quicker. However, we have discovered that the converse is true; they will heal quicker if there is a moist layer under a covered bandage. The only exception is when a wound is excessively draining from the inside, which would require a more absorptive dressing (such as Allevyn).
For proper wound care, clean the wound with saline, apply a topical gel or antibiotic ointment medication to the wound once a day, as recommended by your doctor. After each application, wrap the wound with a clean gauze dressing.
Closely monitor blood sugar levels
Patients with diabetes know how important it is to closely watch their blood glucose levels. This is especially important if you have a foot wound, otherwise known as a diabetic foot ulcer.
When blood glucose levels are high, it prevents our white cells from healing tissues. The high glucose levels can lead to small blood vessel disease and also limit blood flow around the healing process. Without blood flow to heal the wound, it is much like growing flowers without water- it just will not happen.
Reduce the pressure on your foot
The most important aspect of wound healing is “off-loading.” Foot wound care is like the landscaping of newly planted grass; it needs care and time to heal, and in the case of a diabetic foot ulcers, it may require you to be off of your feet. A study of 49 patients in 2017 demonstrated that “while walking may delay wound healing, unprotected standing might be an even more unrealized and sinister culprit.” In particular, the study revealed that standing duration is the only significant predictor of healing at 12 weeks, and is almost three times greater than walking duration in neuropathic foot ulcers.

Preventing diabetic wounds
While diabetic foot ulcers are common for patients with diabetes, they are often avoidable. You can take charge in preventing wounds on yourself or a family member by checking daily for signs like foot trauma, ingrown toenails, sores, bruises, cuts, discoloration and blisters. It may be difficult for you to examine your own foot, so use a mirror or someone for assistance.
Of note, some people may be at a greater risk for diabetic foot ulcers than others if they have:
- Diabetic neuropathy
- Poor circulation
- History of smoking
- High blood sugar
- History of foot deformities (like bunions or high arches)
- Immune-compromising medications (steroids, DMARDs, Humira, Xeljanz etc.)
- Improper shoes
At CFAS wound care centers, our wound care specialist can help manage your risk by providing the necessary equipment and wound care for your diabetic foot treatment.
Wound healing at Certified Foot and Ankle Specialists
The wound care clinics of Certified Foot & Ankle Specialists (CFAS) specialize in treatments for poor-healing and chronic wounds. As a comprehensive wound care clinic, we provide a full assessment, circulation exams, X-rays, specialized treatment, advanced foot wound care healing therapies, grafts (including amniotic stem cell based tissue), patient education and surgery when necessary. Our goal is to heal the diabetic foot ulcer as quickly and painlessly as possible and to eliminate diabetic foot infection and complications; such as scarring and recurrence. We will formulate a diagnosis, and thorough plan to professionally manage your foot wound care.
We have fifteen wound care clinics in South Florida including Broward County (Fort Lauderdale, Coconut Creek, and Coral Springs.) Dr. Rebecca DeSimone, DPM works primarily out of the Fort Lauderdale location on Federal Highway across from Holy Cross Hospital at 4750 N. Federal Hwy, Fort Lauderdale, FL 33308.
Call for an immediate appointment at (954) 561-3338. During the challenging conditions amid COVID-19, we now offer telemedicine and at-home appointments across our offices (please ask the secretary for details).
At Certified Foot and Ankle Specialists, we also treat:
- Sports Medicine problems
- Foot and ankle injuries
- Foot Trauma
- Arthritis
- Work Injuries/ Work Comp
By Dr. Jason LeVitre DPM, FACFAS
Podiatrist and Wound Care Specialist– Fort Lauderdale, Florida
Additions made by Dr. Rebecca DeSimone, DPM
Podiatrist – Imperial Point, Florida