Do you ever find yourself waking up in the morning, stepping out of bed, and getting a sharp pain in your heel/bottom of your foot? Then after walking around for a while, the pain improves. If this is the case, then you may be experiencing plantar fasciitis.
What is HEEL PAIN Plantar Fasciitis?
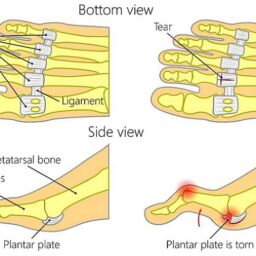
Plantar fasciitis is one of the most common conditions seen by podiatrists. It involves inflammation of the plantar fascia ligament, which originates at the heel and runs across the bottom of your foot to the base of the toes. The most common symptom associated with plantar fasciitis is a sharp pain that presents upon taking the first step out of bed in the morning, or standing up after sitting for a long period of time, with the pain typically subsiding after a period of walking.
This collection of symptoms occurs because the plantar fascia ligament gets shortened at rest and lengthens up when you are walking. Sometimes a heel spur may be identified radiographically in plantar fasciitis patients, however, this is rarely the cause of heel pain plantar fasciitis.
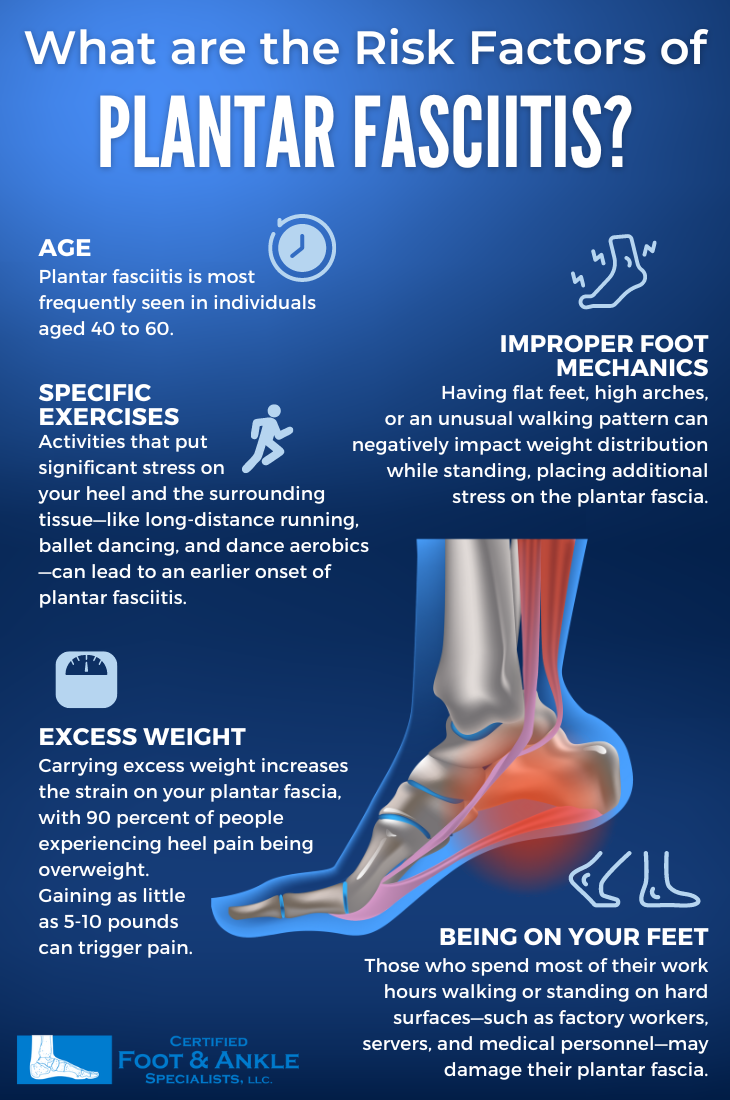
Risk factors for developing Plantar Fasciitis
Plantar fasciitis can affect both athletic and non-athletic patients and typically occurs due to overuse or overstretching of the ligament. Two major risk factors for plantar fasciitis include tight calf muscles and hyperpronation. A lack of flexibility seen with tight calf muscles can result in decreased ankle motion, leading to extra strain being applied to the plantar fascia. With hyperpronation, in which the arch of the foot collapses during weight bearing, the plantar fascia ligament is stretched taut and becomes irritated leading to microtears in the ligament. The body undergoes a continued cycle of tearing and repairing, leading to scarring within the ligament and ultimately resulting in chronic plantar fascia irritation.
Treatment Options
Conservative, non-surgical, treatments for plantar fasciitis are successful the majority of the time. There are a number of treatment options available for this condition including cortisone injections, oral anti-inflammatories, and EPAT (acoustic shockwave therapy). However treatments, such as cortisone injections, are rarely successful in treating the condition alone as the biomechanical component also needs to be addressed. This can be accomplished with plantar fascia and calf stretching in addition to appropriate shoe wear. Avoid barefoot and flat shoes as this results in more pressure being applied to the heel.
Foot Orthotics Are Commonly Overlooked
When additional support is needed, medical grade inserts and custom orthotics are helpful in placing the foot in the appropriate position. We all wear shoes for a large portion of the day and keeping orthotics in our foot wear helps to ensure there is consistency and uniformity. Furthermore, night splints, plantar fascia tapings, and physical therapy are helpful in addressing the biomechanical component of plantar fasciitis. Making sure to use orthotics as you change your shoes, since keeping the foot mechanics consistent is important. Try to choose peer reviewed foot orthotics if choosing over the counter options, this will ensure the right material and purpose is appropriate.
If conservative treatments are unsuccessful, then there are surgical treatments available. The most common surgical procedure is called a plantar fasciotomy, in which one-third to one-half of plantar fascia ligament is released. This may be performed as an open procedure or endoscopically. If present, the heel spur may also be resected.
Nevertheless, our physicians at Certified Foot and Ankle Specialists can determine the best treatment plan for you. Please call one of our local podiatric offices and schedule an appointment today.
By Derek Pawich, D.P.M