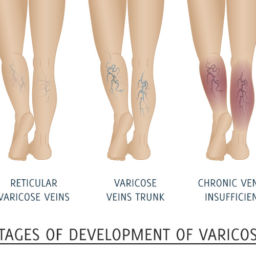
What are spider, reticular and varicose veins?
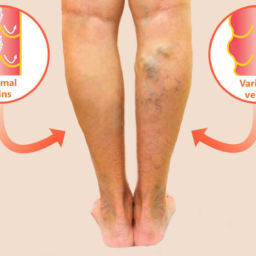
Spider, reticular, and varicose veins are often the first and most visible signs of an underlying long-lasting venous disorder. Their appearance, pattern, position within the different skin layers, and size (diameter) are the main features that define these abnormal veins.
Spider veins or telangiectasias are enlarged blood vessels of less than 1 mm in diameter within the dermal layer of the skin. These veins spread within the skin forming webs of a reddish color. Spider veins are most commonly seen on the face and lower legs.
Reticular veins, also known as venulectasias, are slightly larger and straighter vessels of 1-3 mm caliber, deeper into the skin (subdermal layer), and of a bluish color. Neither spider or reticular veins raise above the skin surface.
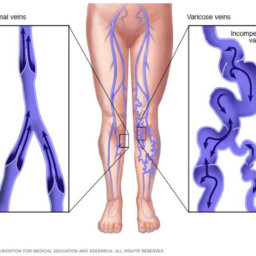
On the other hand, varicose veins are very tortuous (twisted) and palpable veins with a diameter equal or larger than 4 mm. Varicose veins are typically connected to deeper branches (tributaries) off the great saphenous and the small saphenous veins.
How common are these veins?
These are all very common findings in the general adult population. The prevalence of spider and reticular veins in adults is about 60%; whereas, the prevalence of varicose veins is close to 30%- this is considered more common than diabetes mellitus, and comparable to the occurrence of high blood pressure among adults in the United States.
What causes all these veins?
These veins are mostly caused by vein wall weakness at multiple levels, resulting in vein elongation and dilatation followed by valve malfunction and venous reflux (backward blood flow). Valves are small tissue folds inside the veins that allow the blood to flow in just one direction (from the feet back up into the heart).
Genetic (family history) and aging are main predisposing factors for vein wall weakness and valve dysfunction. Damages to the vein wall and the venous valves due to trauma, infection, and blood clots can also result in impaired valve function and reflux. High resistance to normal blood flow due to blockages inside (e.g., blood clots) or outside the veins (e.g., tumors, crossing blood vessels) can cause or contribute to venous hypertension (increased blood pressure inside the vein) in some patients. Calf muscle pump failure due to restricted ankle movement and/or muscle atrophy (muscle wasting) can cause stasis (stoppage or slowdown in the flow of blood), reflux, and venous hypertension. Multiple pregnancies, obesity, chronic lung disease, prostate issues, constipation, and activities requiring prolonged sitting and/or standing contribute to venous reflux and venous hypertension as well.
What are the symptoms?
Most patients with spider and reticular veins have no symptoms. Some patients report discomfort, burning, and itching. Many patients find the appearance of these veins very cosmetically upsetting. A cluster of spider veins around the ankles (corona phlebectatica) is a distinctive clinical marker of a more significant underlying venous problem. Patients with varicose veins usually complain of tenderness along the course of the veins, leg heaviness, fatigue, achiness, swelling, throbbing, and itching. Frequently, they also report leg cramps (Charlie’s horses), restless legs, and skin changes.
What are the potential outcomes?
About 60% of patients with chronic venous disease would experience a progression of their condition later on. More than 30% of patients with just varicose veins will develop skin changes, consequently have a higher risk for ulcers. Nearly 20% of patients with chronic venous insufficiency develop venous leg ulcers. Approximately 50% of healed venous leg ulcers may come back within 10 years. Fifty percent of patients with chronic venous disease in just one leg are expected to develop symptoms and venous reflux in the other initially symptom-free leg at 5 years. Patients with varicose veins have a higher risk of suffering from blood clots in the superficial (superficial venous thrombosis or superficial thrombophlebitis) and deep veins (deep venous thrombosis), bleeding (variceal bleeding), chronic leg swelling and pain, permanent skin discoloration and scarring, and lymphedema (a non-curable condition characterize for a build-up of lymph fluid in the fatty tissues just under the skin).
Do you need to see a doctor?
For most cases, spider and reticular veins are just a cosmetic concern. Patients with corona phlebectatica and symptomatic varicose veins should be evaluated by a physician with formal training and expertise in phlebology (the branch of medicine that deals with veins and their diseases). Our phlebologist (vein specialist) at Certified Foot and Ankle Specialist will meet you and perform a very comprehensive clinical evaluation. Additionally, most patients would have a duplex venous ultrasound (sonography) of their lower extremities done to look for blood clots, blockages, and for the presence, location, and extension of venous reflux.