Wounds on the legs and feet are very common and can sometimes be tough to heal, whether it is a skin tear or a major trauma. Certified Foot & Ankle Specialists are expertly trained in treating wounds on the lower extremities. For patients who may feel discouraged by slow healing wounds or frustrated with bandage changes, here are a few key points regarding wound healing.
Venous insufficiency and Varicose veins
Venous insufficiency can be one contributing factor to slow wound healing as it causes swelling, drainage and skin changes. Varicose veins, heaviness and cramping can be a few signs that you should be tested for this condition. The circulation test to evaluate the veins is an ultrasound. Based on your results, your doctor may recommend compression bandages or stockings and potentially even an in-office procedure to treat the underlying cause of the wound.
Decreased Circulation
Painful wounds on the legs, feet and toes may be caused by decreased circulation. These wounds can take a very long time to heal and tend to be incredibly sensitive. Some people may experience pain in the legs with walking, and may find relief by hanging their feet over the edge of the bed or chair. An ultrasound to assess the blood flow into the feet and legs is a baseline study done in office to evaluate for blockages that might need further treatment.
Nutrition
Nutrition plays a very important role in overall health, but even more so when a patient has a wound. Diets with increased amounts of protein are important to promote healing. Adding protein in the form of a shake or drink supplement is also a good option to speed up healing. Regular blood work can show vitamin deficiencies that can also lead to slow wound healing.
Diabetic Patients and Wounds
Diabetic patients with wounds are a special group who have other risk factors that may delay wound healing. When a diabetic has a wound, blood flow studies must be performed to evaluate for poor circulation (this is a very common reason for slow wound healing.) With reduced blood flow, the growth factors needed for healing are not able to go to the area of the wound.

Patients with diabetes are at an increased risk of infection with slowed wound healing due to immune system changes that must be monitored. Wound cultures are swabs taken from the wound to determine if bacteria is growing for the correct antibiotic to be prescribed. Infected ulcers may require more aggressive treatment such as cleaning out the infection in the office.
The sooner wounds can be treated, the better chance of preventing the spread of infection. Regular wound care with a podiatrist, cleaning and bandaging of the wound are key steps in wound healing.
Calluses on Diabetic Patients
Changes in the feet are common with diabetes including foot deformities such as hammer toes and changes in the arch. These changes in the bone can cause calluses that can ultimately turn into wounds if not treated. Callus shaving is a large part of diabetic foot treatment that is performed on a regular basis in the podiatry office. Diabetic patients should be using diabetic shoes and special inserts to prevent calluses and pressure points. Insurance companies do typically cover these preventive devices.
Skin Changes
Skin changes on the feet are another finding seen with diabetes. The skin may become dry, flaky and crack which can cause a wound and possibly an infection. Moisturizing the bottoms of the feet with a diabetic foot cream each day will soften the skin and prevent the skin from drying out. Water after a shower or sweat can trap moisture between the toes also resulting in possible infections. Cleaning the feet carefully with soap and water and drying between toes will prevent this issue.
Peripheral Neuropathy
Up to one half of all diabetic patients experience peripheral neuropathy symptoms. Neuropathy can present as numbness or with different sensations such as tingling or burning or “ants crawling” on the legs and feet. This nerve damage from high blood sugar levels depends on factors such as type 1 or type 2 diabetes, how long a patient has had diabetes, blood sugar levels and nutritional status. A major concern for patients with diabetes is developing a wound due to the absence of feeling in the feet. One of the main goals in diabetic foot treatment is to decrease risk factors and prevent foot issues and wounds. A nerve study may be recommended to evaluate for neuropathy.
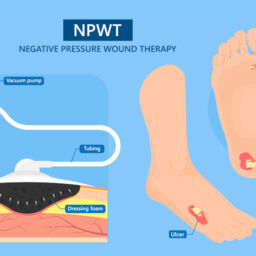
Bandaging up a Wound
Once a wound develops on the foot or the leg, evaluation, wound care and guidance is needed from a podiatrist who specializes in the leg and foot. Diabetic foot treatment for wounds includes cleaning the wound, applying medicated ointments and creams and applying special bandages to promote wound healing.
One of the bandages used in diabetic wounds is a total contact cast. A total contact cast is a special fiberglass cast that is used specifically in diabetic foot treatment for wound healing. This type of wound care bandage is safe for patients with neuropathy and is the gold standard treatment for diabetic foot wounds. The cast is padded around bony prominences to take the pressure completely off the pressure points for the ulcer to heal.
Monitoring and Check-Up Appointments
For people with diabetes, checking blood glucose daily at home is the best way to manage blood sugar levels and decrease the risk of complications from diabetes. Regular check-up appointments with your primary doctor, your endocrinologist and your podiatrist are extremely important for checking blood work and making changes to medications when needed as well as prevention of issues such as diabetic foot problems. The doctor may recommend special shoes and inserts as well as vitamins for neuropathy. Daily self-exams at home to inspect the feet are a critical step in preventing wounds.
If a wound develops, make an appointment with your podiatrist as soon as possible to examine the wound carefully; early treatment helps decrease the risk of infection. Telemedicine has also become a great new supplement to treatment that has made access to doctor appointments much easier and convenient for patients. If you have been recommended for an amputation, do not proceed until you have had a second opinion from one of our specialists. We save limbs!
Make an in-office or telemedicine appointment with one of specialists today at 855-317-5080.